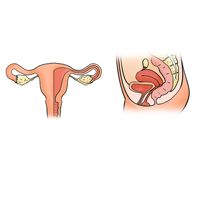
Is pelvic organ prolapse correction with vaginal mesh suitable with a correct indication and protocolized follow-up?
Submitted: 12 November 2021
Accepted: 25 January 2022
Published: 14 February 2022
Accepted: 25 January 2022
Abstract Views: 1608
PDF: 411
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- Maxime Marcelli, Gilles Karsenty, Jean-Philippe Estrade, Aubert Agostini, Ludovic Cravello, Gérard Serment, Marc Gamerre, Factors influencing sexual function in women with genital prolapse , Urogynaecologia: Vol. 25 No. 1 (2011)
- Dorota Borawski, Martin H. Bluth, Wellman W. Cheung, Prevalence of urinary incontinence and other lower tract urinary symptoms in patients with uterine myomas , Urogynaecologia: Vol. 25 No. 1 (2011)
- Chendrimada Madhu, Penelope Harber, David Holmes, Unexpected benefits and potential therapeutic opportunities of tension free vaginal tape for stress urinary incontinence , Urogynaecologia: Vol. 27 No. 1 (2013)
- Nisarath Soontrapa, Sukree Soontrapa, Srinaree Kaewrudee, Woraluk Somboonporn, Chuanchom Sakondhavat, Urogenital symptoms in postmenopausal women: a hospital-based prevalence study , Urogynaecologia: Vol. 25 No. 1 (2011)
- Xiao Luo, Li Xiao Wan, Hong Shen, Yin Xiu Xia, Chao Han Zhang, Yi De Luo, Yi Dai, Jia Wang, Pregnancy after tension-free vaginal mesh (anterior Prolift) and concomitant tension-free vaginal tape-obturator procedure , Urogynaecologia: Vol. 25 No. 1 (2011)
- Kristina Crafoord, Jan Brynhildsen, Olof Hallböök, Preben Kjølhede, Pelvic organ prolapse and anorectal manometry: a prospective study , Urogynaecologia: Vol. 26 No. 1 (2012)
- F. Bernasconi, V. Napolitano, M. Primicerio, D. Lijoi, E. Leone, F. Armitano, M. Luerti, G.C. Sugliano, D. Vitobello, D. Riva, D. Gregori, SUI AND TVT IUS ND TVT SECURE SYSTEM: A PROSPECTIVE OBSERVATIONAL MULTICENTRIC STUDY. MORBIDITY AND SHORT-TERM PERCENTAGES OF SUCCESS , Urogynaecologia: Vol. 23 No. 3 (2009)
- Ali Mahmood, Prianka Gajula, The role of the urogynecologist with sphincteroplasty: a multidisciplinary approach to a very common, yet devastating problem , Urogynaecologia: Vol. 26 No. 1 (2012)
- N. SEBASTIO, M. SIMONAZZI, E. FERRI, S. MELI, P. SALSI, P. CORTELLINI, Profile of the urethral transmission pressure in patients undergoing tension-free vaginal tape (T.V.T.) , Urogynaecologia: Vol. 14 No. 1 (2000)
- Khaled Refaat, Constanze Fischer-Hammadeh, Mohamad Eid Hammadeh, Overview of pelvic floor failure and associated problems , Urogynaecologia: Vol. 26 No. 1 (2012)
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/uij.2022.280
https://doi.org/10.4081/uij.2022.280



