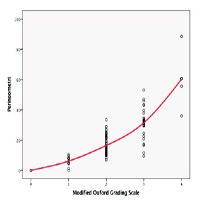
Correlation of levator ani muscle strength measurement between Modified Oxford Grading Scale and perineometer on pelvic organ prolapse patient
Submitted: 28 February 2021
Accepted: 15 June 2021
Published: 30 June 2021
Accepted: 15 June 2021
Abstract Views: 2514
PDF: 279
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- J. BECO, J. MOUCHEL, PERINEOLOGY: A NEW AREA , Urogynaecologia: Vol. 17 No. 2 (2003)
- V. Leanza, N. Gasbarro, S. Caschetto, NEW TECHNIQUE FOR CORRECTING BOTH INCONTINENCE AND CYSTOCELE: T.I.C.T. (TENSION-FREE INCONTINENCE CYSTOCELE TREATMENT) , Urogynaecologia: Vol. 15 No. 3 (2001)
- F. Bernasconi, G. Pisani, G. Orfanotti, S. Arienti, G. Marelli, EPIDEMIOLOGY OF THE LOWER URINARY TRACT DYSFUNCTIONS IN THE FEMALE DIABETIC POPULATION , Urogynaecologia: Vol. 15 No. 3 (2001)
- Vineet Mishra, Smit Solanki, Rohina Aggarwal, Athulya Shajan, Patients with transobturator tape: a retrospective observational study of ten-year follow-up , Urogynaecologia: Vol. 36 No. 1 (2024)
- Carlo Rappa, Gabriele Saccone, Efficacy of the inside-out tramsobturator tension-free vaginal tape (TVT-ABBREVO) for the treatment of stress urinary incontinence after a 12-month follow-up , Urogynaecologia: Vol. 30 No. 1 (2017)
- Sujatha Narayanamoorthy, Kimen Singh Balhotra, Michael Silver, Rodney McLaren Jr., Elishia McKay, Residents’ experience and training in obstetric anal sphincter injury repair in the United States , Urogynaecologia: Vol. 35 No. 1 (2023)
- Daniele Porru, Enrica Bucchioni, Marcello Macchi, Fabio Leva, Alberto Parmigiani, Davide Barletta, Dimitrios Choussos, Barbara Gardella, Maria Diletta Daccò, Rossella Elena Nappi, Massimo Allegri, Carlo Maria Bianchi, Arsenio Spinillo, Bruno Rovereto, Explorative study on the use of omalizumab in patients suffering from interstitial cystitis/bladder pain syndrome , Urogynaecologia: Vol. 26 No. 1 (2012)
- Zhuoran Chen, Lucy Bates, Nevine Te West, Kate H. Moore, A 9-year audit of the efficacy of diathermy for cystitis cystica , Urogynaecologia: Vol. 31 No. 1 (2019)
- Abdullahi Khalid, Abdullahi Alhassan, James Oche Ejembi, Abdullahi Abdulwahab-Ahmed, Atypical presentation of vesicouterine fistula (Youssef’s syndrome) post-caesarean gossypiboma: a case report , Urogynaecologia: Vol. 35 No. 1 (2023)
- Pattaya Hengrasmee, Parit Wachasiddhisilpa, Chutimon Asumpinwong, Pichai Leerasiri, Outcomes of colpectomy for uterovaginal and posthysterectomy vault prolapse: A comparative study between normal and overweight women , Urogynaecologia: Vol. 31 No. 1 (2019)
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/uij.2021.268
https://doi.org/10.4081/uij.2021.268



